Meeting the Metrics: How Interventional Cardiologists Are Maintaining PCI Proficiency in Rural America
Choosing to practice in rural America has its benefits and challenges. While some interventional cardiologists may be concerned that they won’t be able to meet the yearly percutaneous coronary intervention (PCI) proficiency quota necessary to maintain their credentials, many are finding more than enough volume in underserved areas. In fact, interventional cardiologists practicing rurally aren’t just surviving but thriving, applying their skills in a more meaningful way.
The State of Cardiac Care in Rural America
The rate of cardiovascular disease is 40 percent higher among rural Americans as compared with those living in urban areas. Rural residents are more likely to die from heart disease and stroke. Patients receiving treatment for acute myocardial infarction at rural hospitals have lower rates of cardiac catheterizations, PCIs and coronary artery bypass grafts compared with those treated at urban centers.
With an estimated 60 million people living in rural America, these trends are concerning as disparities in access and outcomes continue to compound these issues.
Despite a demonstrated need for comprehensive cardiac care, there is a shortage of specialists like cardiologists in these areas. Understandably, this lack of access contributes to poorer outcomes and a reduced life expectancy.
Meeting Performance Metrics
A PCI is any non-surgical procedure used to treat the blockages in a coronary artery. PCIs open narrowed or blocked sections of the artery to restore blood flow to the heart. Interventional cardiologists must perform at least 50 PCIs a year to maintain their credentials and board certification. Depending on the state, the hospital may suspend a physician’s privileges if this threshold is not reached or grant a waiver to allow the clinician to continue to practice on a limited basis.
Evolution of PCI Volume Standards
In the early days of performing PCIs, it was believed that the higher the volume, the better the outcomes. In 1993, the American College of Cardiology (ACC) and the American Heart Association released guidelines recommending that each operator complete a minimum of 75 angioplasties each year. The ACC further recommended a minimum annual threshold of 400 PCIs per hospital in 1998. In 2013, as more physicians mastered the procedure, the annual PCI quota per operator was reduced to 50, averaged over two years.
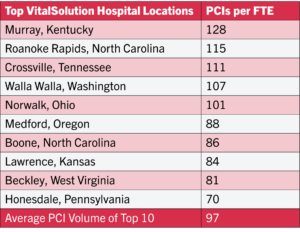
VitalSolution primarily serves rural and regional hospitals. Facilities contracted with the group currently average 78 PCI procedures per full-time equivalent (FTE) physician. Perhaps even more impressive, the practice’s top 10 highest-volume clients average 97 PCIs per year per FTE.
Addressing Recruitment and Caseload Challenges in Rural Settings
Our medical staff handles a caseload that’s in the top 20 percent in volume in the country, but recruiting clinicians to this area is difficult.
Joel Wassermann, MD
Providence St. Mary Medical Center is a VitalSolution client in Walla Walla, Washington. The 100-bed hospital is located in a city of 34,000. The next largest metropolitan area is the “tri-cities” of Kennewick, Pasco and Richland—about an hour away.
“Volume here is pretty high,” says Joel Wassermann, MD, the hospital’s chief medical officer. “Our medical staff handles a caseload that’s in the top 20 percent in volume in the country, but recruiting clinicians to this area is difficult. While we’re in the largest city in the area, we’re isolated.”
These conditions aren’t limited to the Pacific Northwest. Shriti Masrani Mehta, MD, is an interventional cardiologist at East Carolina University (ECU) Health Hospital North, a 204-bed regional hospital in Roanoke Rapids, North Carolina. She joined VitalSolution in 2023 after her family moved to North Carolina from Orlando, where she had a large, well-established practice.
The staff in the cath lab at ECU sees a variety of cardiac conditions, from coronary disease and peripheral vascular disease to calcified arteries and complex cardiac lesions. When it came online in 2021, the lab saw about 80 PCI cases. It added a second cath lab in 2023 and plans to increase its volume to 175 in 2024. Dr. Mehta shares this caseload with one other interventional cardiologist. On a typical day, she rounds on 10 to 15 inpatients.
Because there are fewer cardiologists at ECU, it’s easier to get enough procedures to meet the requirement.
Shriti Masrani Mehta, MD
“Because there are fewer cardiologists at ECU, it’s easier to get enough procedures to meet the requirement,” she says. “When I’m working, I’m the only doctor. I’m not splitting the volume with several other physicians.”
“Maintaining volume isn’t a concern,” adds Jasdeep Dalawari, MD, FACC, FSCAI, who also practices at ECU Health Hospital North. “It’s very doable, and if the numbers aren’t trending in the right direction, you can supplement your caseload at another facility in the area. The company is always looking at the numbers and acts quickly if someone is in danger of not making their quota.”
Building a Resilient Cardiology Practice
Three years ago, after practicing medicine in the U.S. Navy for 20 years, Bradley Serwer, MD, joined VitalSolution at Wayne Memorial Hospital, a 90-bed community hospital in Honesdale, Pennsylvania. In addition to the generations of families who have called the blue-collar mountain region home, the area has seen a recent influx of newcomers in the wake of the COVID-19 pandemic.
“We see the entire gamut of the healthcare spectrum,” Dr. Serwer explains. “Some of the patients we see have only sought care because of an overt emergency. They have neglected preventive medicine and screening exams and now find themselves with an acute cardiac issue that requires emergency treatment.”
WMH’s cardiac catheterization program started in 2016 and has seen its volume grow each year. It contracted with VitalSolution in 2019 after its sole interventional cardiologist left the organization. The hospital performed 125 PCIs in 2023, with the workload shared between two interventionalists. It aspires to grow its volume to 200 PCIs annually.
A Sustainable Practice Model in Cardiology
I was going to join a private practice, but because there are too many interventionalists in the region I would’ve had to cover four hospitals to meet the PCI requirement.
Brad Serwer, MD
Home for Dr. Serwer is in Bethesda, Maryland, a suburb of Washington, D.C. When he retired from the Navy and sought employment as a civilian, he learned that the region was “saturated” with interventional cardiologists. He was concerned that he wouldn’t be able to meet the annual PCI performance threshold.
“I was considering joining a private practice in the Washington, D.C. area, however, this is an area that is saturated with interventional cardiologists. I was going to cover four hospitals and spend much of my time in the car. It just wasn’t a good use of my time,” he says. “When I heard about VitalSolution’s model, it seemed too good to be true. I worried that the volumes in rural communities just weren’t high enough. I’ve been pleasantly surprised. I’ve always maintained the right caseload without working additional shifts.”
If volumes are low, VitalSolution’s leadership team helps physicians find ways to boost their caseload.
“Volume numbers are evaluated monthly, and the whole team supports you if volumes aren’t trending positively,” explains Dr. Dalawari, who also serves as regional chief medical officer for VitalSolution. “There are provisions that enable physicians to visit another site to perform additional procedures. You’re not alone; maintaining proficiency is as important to the company as it is to you. We’ll make it a priority to get you those numbers.”
The Rewards of Going Rural
Established in 2011, VitalSolution’s mission is to reshape healthcare by delivering tailored cardiovascular and anesthesiology services to hospitals nationwide. The physician-led company believes that access to quality healthcare is a right, not a privilege. Its innovative practice model attracts highly trained and accomplished interventional cardiologists through a competitive pay package and built-in work-life balance.
The benefits of this type of work model are plentiful.
Work-Life Balance
Our model is ideal because patient volumes have increased and cases have gotten more complex.
Jasdeep Dalawari, MD
Dr. Serwer, who also serves as chief medical officer at VitalSolution, covers the cath lab at WMH for seven days and then is off for seven days. When it’s time to report for his shift again, he drives four hours from Maryland to Pennsylvania. He meets the other interventional cardiologist at noon on Monday to receive the handoff report.
“When you’re off, you’re completely off,” Dr. Serwer says. “The cardiologist who’s on takes all of the calls. You can turn off your phone, go on vacation and take time to recharge. You can be fully present at home, take the kids to school or see their games. You may still miss some events, but you’ll miss a lot less than if you were working a traditional job.”
Dr. Dalawari, who joined VitalSolution after 10 years in private practice, was drawn to the company’s flexible model.
“Our model is ideal because patient volumes have increased and cases have gotten more complex,” he says. “It’s become harder to maintain focus and stay fresh. In a traditional private practice, you might get two weekends off a month if you’re lucky. It’s hard to refresh your energy in so little time.”
Serving the Underserved
“It’s rewarding to work in an underserved area where your presence truly makes a difference. There aren’t 40 other Interventional Cardiologists fighting over patients,” Dr. Serwer says. “You know your value here. You know that what you do matters, and you feel the appreciation from your patients, administrators and colleagues.”
“When you practice in a major city, you become just a cog in the wheel. It’s like you’re a factory worker, punching in and out, making widgets,” Dr. Dalawari adds. “In rural areas, patients are a lot more appreciative. Without you, they would have to travel quite a distance to see someone else. Instead, you’re treating the Wal-Mart clerk or the waiter at the local restaurant. The doctor-patient relationship has suffered in urban centers, but in rural areas, it’s thriving.”
Dr. Wassermann agrees, “Clinicians here have a sense of duty to the community. We’re not anonymous here. We see our patients out in the community. Other hospital administrators talk about serving their communities, but it’s just rhetoric. Here, it’s real.”
Improved Communication
For Dr. Wassermann, another perk of practicing rural medicine is that a smaller medical staff often makes communication among providers easier.
“Our medical staff is small enough to communicate well with each other,” he says. “We’re not just colleagues; we’re all part of a small institution. It’s easier to communicate, and we’re more agile to address problems.
Improved Access to Cardiac Care
Without adequate interventional cardiology services locally, rural residents must travel long distances or forgo care. If there weren’t an interventional cardiology program at ECU, patients would need to travel up to two hours for care.
“Even transferring a patient to another facility takes a lot of time, and other area hospitals are often at capacity,” Dr. Mehta says.
The same is true in Walla Walla and Honesdale, where the weather can complicate patient travel or transfer.
Striking the Right Balance
Interventional cardiologists across the country are finding meaningful work in underserved areas while still keeping their skills sharp and maintaining their procedural proficiency.
Rural medicine is this hidden gem where you can go back to the basics and what really matters: the doctor-patient relationship.
Jasdeep Dalawari, MD
“I was excited when I saw that VitalSolution averages nearly 80 PCIs per physician. It really is possible to maintain proficiency while working only every other week,” Dr. Serwer says. “We can attain work-life balance and keep our credentials while doing important work in a geographically disadvantaged region. It’s one thing to work in medicine, but it’s especially rewarding knowing that you’re providing care that would not be delivered if you weren’t there.”
For Dr. Dalawari, taking a step back and working less has given him and his patients much more.
“Doctors nationwide are being pressured about metrics, financials and efficiency. Rural medicine is this hidden gem where you can go back to the basics and what really matters: the doctor-patient relationship,” he says. “The need for cardiologists in rural areas is great. You can make a big impact there without sacrificing your income or volume. From almost every perspective, working in a rural area is better than working in other locations.”
To learn more about VitalSolution’s unique program model, contact us today.
 company
company 
 (866) 755-7519
(866) 755-7519